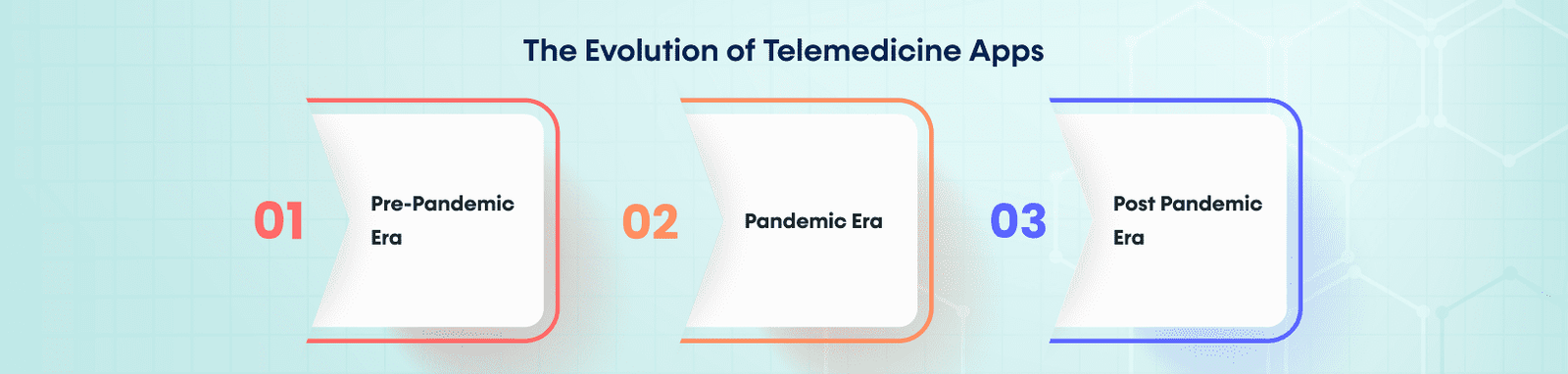
The era following COVID-19 has seen a lot of changes. A lot of things have become virtual. Healthcare is one of them.
Studies show that there has been a stark increase in the use of telehealth apps. Studies by McKinsey also have similar findings. It shows that the use of telehealth has stabilized at 38 times higher than in pre-pandemic times.
But just having an app does not save your back. It has to be ready to adapt to the new trends. It should be able to handle the challenges of the times.
Telemedicine apps and virtual visits are the new normal. Customer needs are changing too. The app you choose should serve both the customers and healthcare providers.
In this article, we will look at how Telemedicine apps prepare you for the future of remote healthcare.
Telemedicine Apps Empowering Healthcare Providers
The COVID lockdowns were nothing short of a nightmare. It affected those in need of healthcare. The healthcare providers were also hit.
It was technology that saved the day. With lockdowns and people stuck in their homes, they could not access necessities. With different apps, we got virtual access to these.
This technology is still available after the pandemic. This opens up new prospects for the healthcare industry. With more access and benefits, these apps have much potential to explore.
6 Key Benefits of Telemedicine Apps
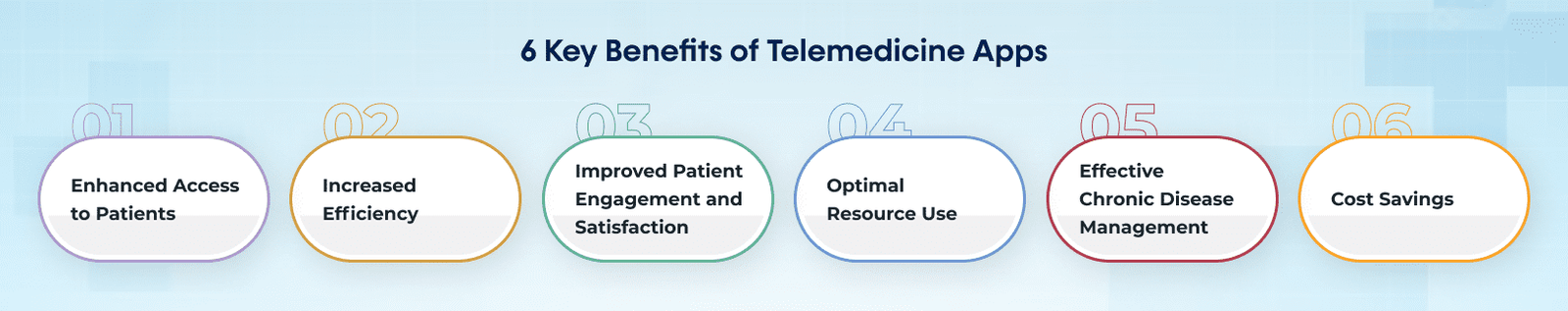
1. Enhanced Access to Patients
The app brings the doctor and patient onto the same platform. Even if they are miles apart. It can help provide access to remote areas.
Someone may need a specialist to assess them. Such a facility may not be available in their place. It can be solved with this technology.
For Instance, Doctor on Demand is a popular telemedicine app. It provides virtual visits to doctors. The app has reduced the number of emergency room visits.
2. Increased Efficiency
With this technology in tow, work becomes more efficient. Healthcare providers can manage time better. Their resources are also used more efficiently. They can do most of the work online.
3. Improved Patient Engagement and Satisfaction
Thanks to these apps, patients can be in direct contact with doctors and nurses. The patient can stay in touch with them and get advice and help when needed. This increases their satisfaction.
A study shows that people who use these apps are more satisfied. 851 people out of 1000 people surveyed said they were happier with the service.
4. Optimal Resource Use
With these apps in tow, healthcare providers can use their resources better. Since a lot of the patient meetings are virtual, they can put aside these resources for urgent ones.
5. Effective Chronic Disease Management
Patients with chronic illnesses can benefit from these apps. Doctors can keep an eye on them and manage their conditions better. The doctor can track vital signs and give advice. They can also give better treatment plans.
Teladoc, a popular app, showed the positive impact of this tech. It was able to help manage diabetes, blood pressure, and rheumatoid arthritis better.
6. Cost Savings
In-person visits involve a lot of expenses. Using virtual meetings saves a lot of money for both the doctor and the patient. Travel expenses are also cut. The clinic or hospital is also not weighed down. Research conducted by Geisinger Health Plan proves this. The use of virtual apps resulted in 11% cost savings.
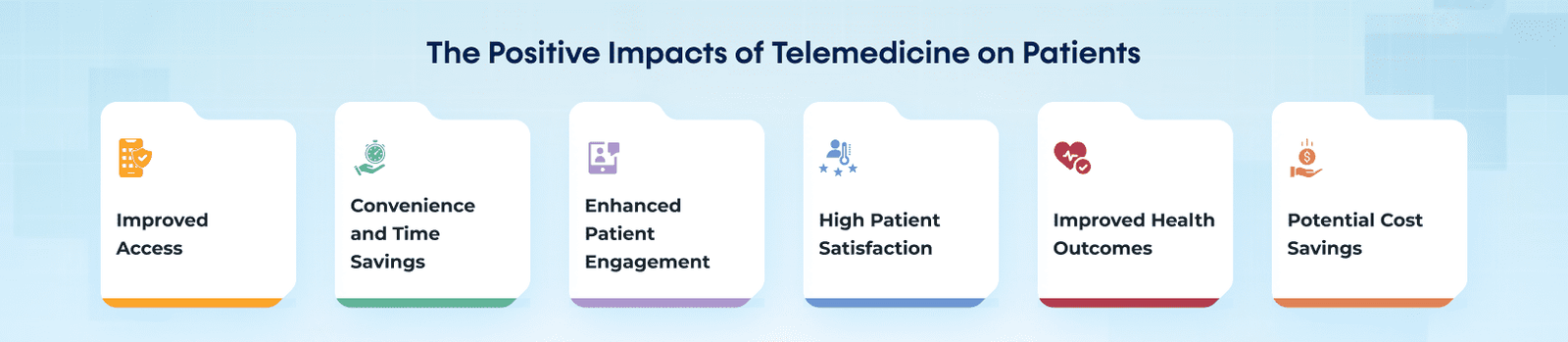
The Positive Impacts of Telemedicine Apps on Patients
The use of telemedicine apps has changed the way patients engage with healthcare facilities. Let us look at the positive impact these apps have on patients.
Improved Access
The use of apps brings down the walls between people. Medical help is now accessible to patients wherever they are.
A survey conducted in March 2021 proves this. It showed that 86% of Americans found it easier to access a doctor through telemedicine.
Convenience and Time Savings
Patients can receive medical care from the comfort of their own homes. They can save time and money as they don’t have to travel to clinics. They don’t have to spend time waiting either.
Using the app, around 63% of patients felt this way. They were comfortable and convenient.
Enhanced Patient Engagement
With technology by their side, patients are involved in their healthcare journey. They can keep track of their health. It gives them more control over their healthcare journey.
High Patient Satisfaction
Patients using telemedicine services report high levels of satisfaction. It is easier for them in many aspects.
A large number of patients (67%) said they preferred it over in-person meetings.
Improved Health Outcomes
The use of these apps leads to healthier people. As people are more aware of their health, they are more active.
Telemedicine consultations increase positive health outcomes. It leads to better health across various medical specialties.
Potential Cost Savings
Patients can reduce the amount of money they spend on their health by choosing this app. There is no need to visit the ER for every small thing. They can contact the provider and get help when necessary.
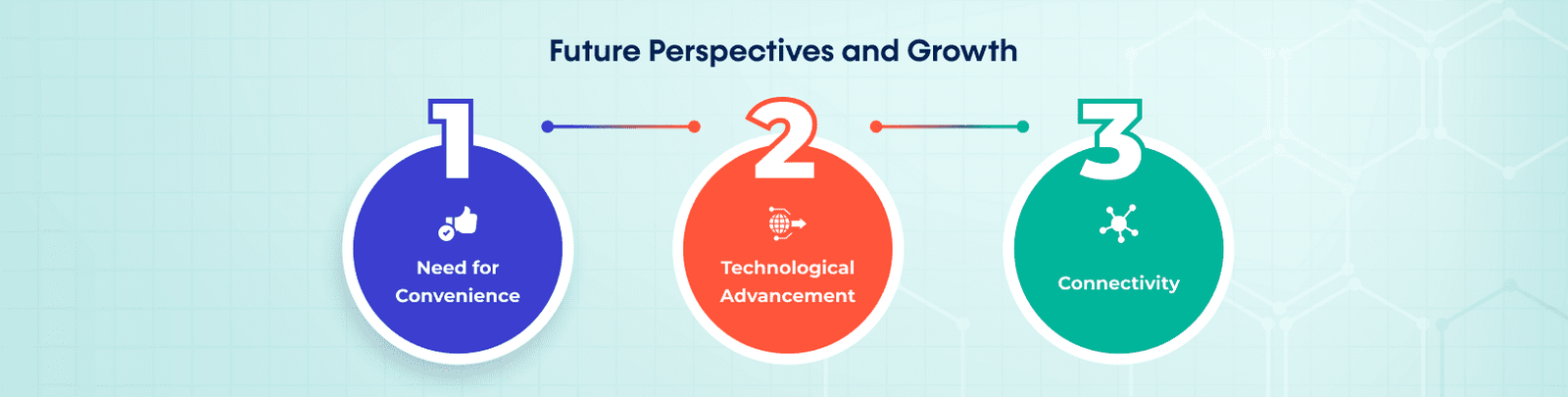
The Future Of Telemedicine
Healthcare providers, as well as patients, stand to gain from this tech. One can safely say that it is here to stay. It holds great promise for the future.
The telemedicine market is expected to grow at a CAGR of 12.20%. The market value is expected to reach US$36.126 billion by 2026.
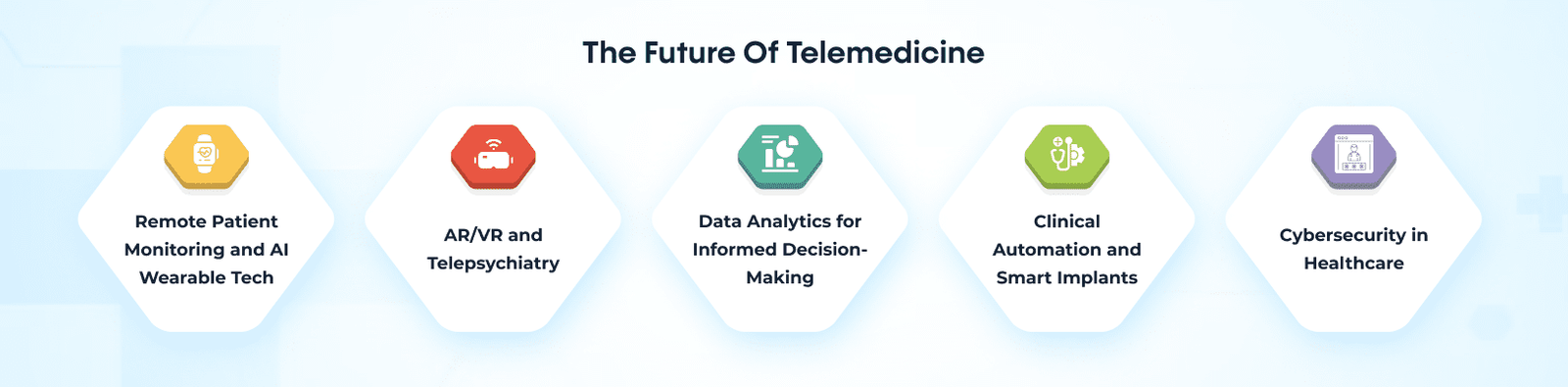
Here are some of the advancements shaping the future of healthcare:
Remote Patient Monitoring and AI Wearable Tech
AI and the healthcare Internet of Things (IoT) wearable technology are bringing in waves of changes. One instance of it is Remote Patient Monitoring (RPM). It helps providers keep an eye on the patient. It also improves patient outcomes and reduces costs.
AR/VR and Telepsychiatry
Augmented Reality (AR), Virtual Reality (VR), and telepsychiatry hold promise for the future. They give immersive experiences. Users can learn many useful things from it. They help remote meetings and improve access to mental health support.
Data Analytics for Informed Decision-Making
Healthcare Data analytics can help predict health outcomes. Providers can make informed decisions for personalized treatment plans. It can help improve patient care and identify trends. It will also make healthcare delivery better.
Clinical Automation and Smart Implants
Clinical automation and the use of smart implants is another possible tech. It can enhance patient safety and reduce errors. It also decreases the delays in healthcare delivery.
Automation improves the work of healthcare providers. With it, they can give accurate and real-time service. With smart implants, patients can get custom and specific treatments.
Cybersecurity in Healthcare
Cybersecurity has become a top concern in protecting sensitive medical data. It helps maintain privacy and prevent data breaches.
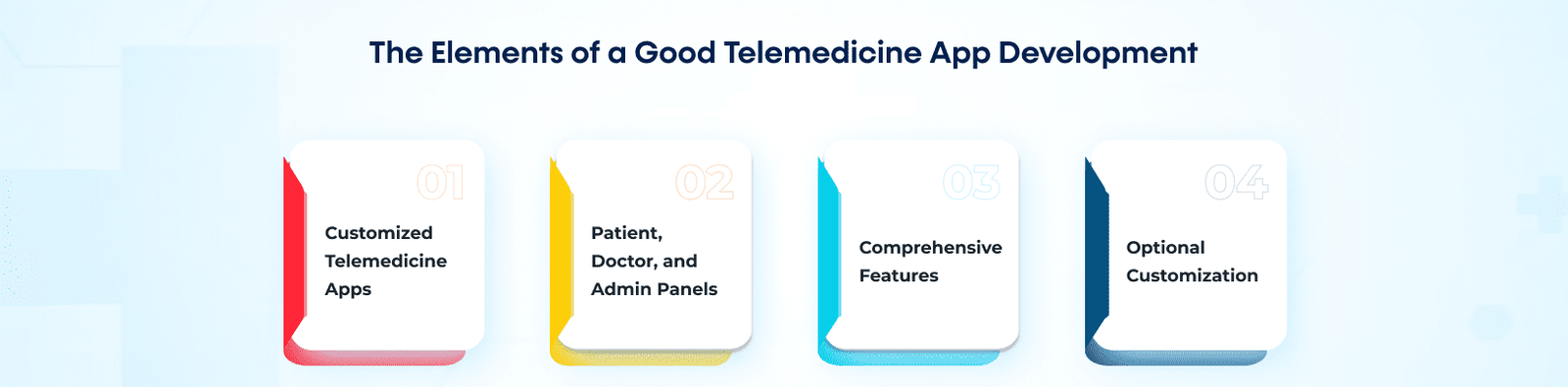
The Elements of a Good Telemedicine App Development
If you are planning to invest in a telemedicine app, here are some things you need to look out for.
EMed HealthTech is a leading telemedicine app development company. We offer complete solutions suited to your needs. Let’s take a look at the services and the key features we offer.
Customized Telemedicine Apps
EMed HealthTech focuses on developing white-label and customized telemedicine apps. The apps are made to suit the unique needs of doctors, hospitals, and clinics.
Patient, Doctor, and Admin Panels
EMed HealthTech’s apps include separate panels for patients, doctors, and admins. They provide a range of different features to use. The interfaces are made such that there are smooth interactions.
Comprehensive Features
EMed HealthTech offers a range of features in its apps. This includes:
- Appointment scheduling
- Video calls
- Secure Messaging
- Electronic health records (EHR)
- Prescription management
- Payment processing.
These features offer convenience and ease of access.
Optional Telemedicine App Customization
EMed HealthTech provides optional custom features. Providers can tailor the apps to suit their specific needs. This means that every user gets a different experience.
Our telemedicine app developers first take account of your needs and budget.
Ready to Step into the Future of Digitized Healthcare with Telemedicine?
Telemedicine app development is changing healthcare. It offers better access, convenience, and patient engagement. In the post-COVID era, one thing has become very clear: Technology and remote healthcare play a major role in the future of healthcare.
Traditional healthcare models are no longer suitable for today’s world. The rise of technology has transformed the approach to medical care.
If you are a healthcare provider that wants to succeed, EMed HealthTech is the answer you are looking for.
EMed HealthTech is ideal for customized telemedicine app development services.
Contact us today to discuss how our expertise can help you.