The delivery of healthcare services has changed as a result of the quick development of digital health technology. Its growth has revolutionized patient care by creating a bridge between healthcare providers and patients, and it has enabled the delivery of consultation, diagnosis, and treatment without being physically present. Telemedicine technology has made accessing medical services more convenient and time-efficient than ever.
In this article we cover how these telemedicine apps are transforming the healthcare domain, what are the benefits of using the telemedicine app and the key elements of telemedicine software solutions that help bridge access to healthcare.
Discovering the Telemedicine App!
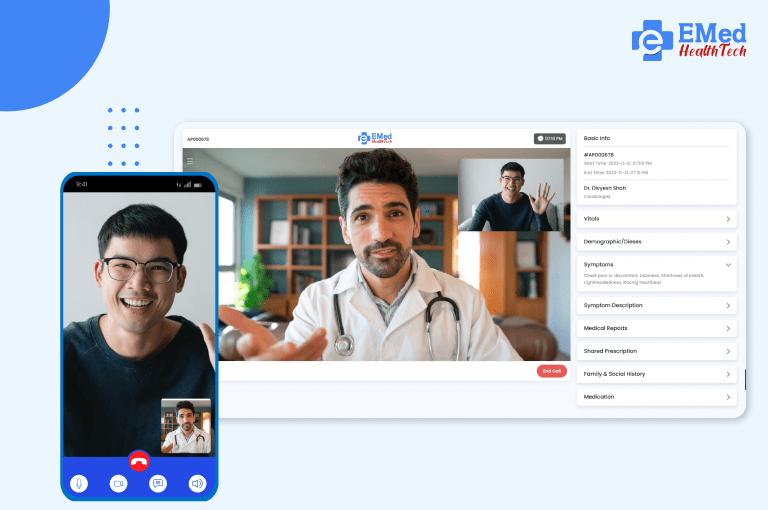
A telemedicine app is a website or mobile application that enables a virtual consultation with a doctor. These apps enable patients to reach out to healthcare professionals instantly via video calls/chats/voice calls and receive medical advice without the need for a visit to a clinic/hospital. From EHR to appointment bookings and e-prescriptions, these platforms have been created to make healthcare services accessible and efficient.
Telemedicine App Development in Modern Healthcare
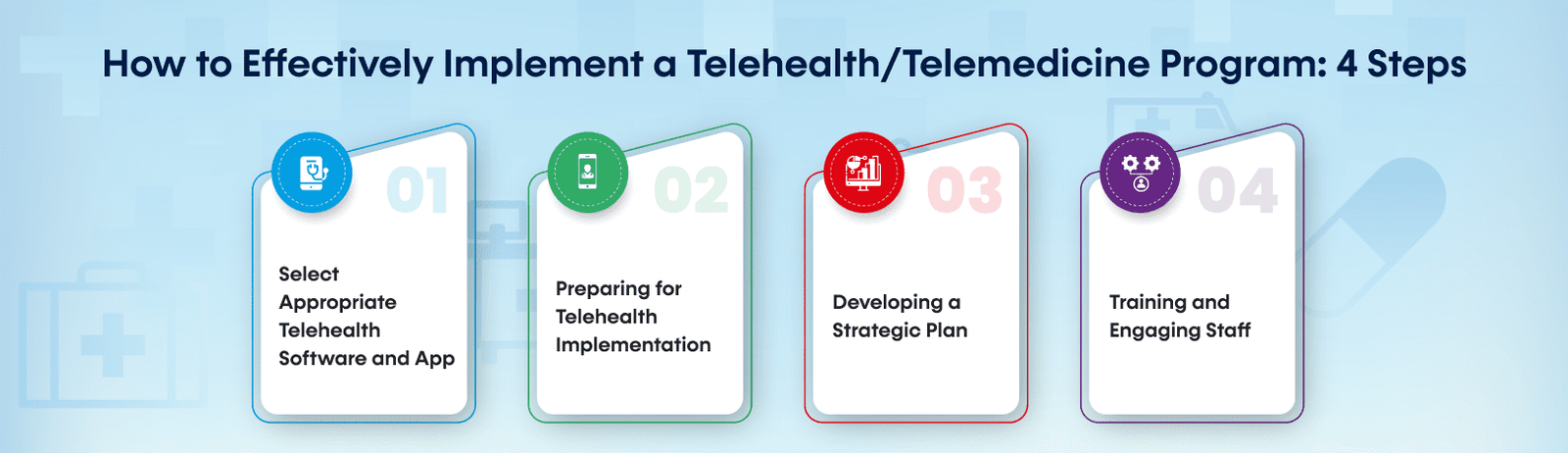
Telehealth apps go in line with these concerns, helping make healthcare services more patient-centric. Healthcare services have a remarkable expansion due to the rise in chronic diseases, increasing patient footfall, and the sustainability of remote care solutions, thus telemedicine software solutions come as a hero to enhance healthcare accessibility and efficiency.
Here are a few things telemedicine development changes in healthcare:

- Improved Accessibility: Telemedicine helps patients living in remote areas to get medical services without travelling.
- Savings on Time and Cost: The reduction in physical visits also facilitates savings in the time taken and the medical expenses.
- Reduced Burden on Hospitals: Virtual consultations help hospitals manage the flow of patients.
- Improved Management of Chronic Disease: The telemedicine segments will allow for better patient management.
- Improved Patient Engagement: Patients can consult doctors during the day or night, improving their well-being.
Important Features Of A Telemedicine App
Essential elements that expedite virtual healthcare services are necessary for a telemedicine app to be successful. Among the essential characteristics are:

-
User-Friendly Interface
A telemedicine platform can work only when it has a defined user experience in both patients’ and doctors’ wings. Easy access is important to make sure frictionless interaction is happening.
-
Having Consultations Via Video & Audio Securely
High-quality video and audio calls are paramount for successful remote consultations. They comply with HIPAA and employ encrypted channels to safeguard patient data.
-
Appointment Scheduling And Management
Make it easy for patients to book, reschedule or cancel appointments. Automation of notifications and reminders generates a record that helps to reduce missed consultations.
-
Integrations With An Electronic Health Record (EHR)
A telemedicine app needs to integrate with EHR systems so that it has access to the medical history, prescriptions, and lab reports of the patients.
-
Online Pharmacies and E-Prescription
Doctors can generate electronic prescriptions, and patients can order medicines through an inbuilt pharmacy service in the app.
-
AI-Powered Chatbots for Initial Screening
Comment: Pre-diagnosis: AI-powered chatbots help in collecting patient symptoms pre-diagnostic and guide towards the desired specialist.
-
Multi-Device Compatibility
This means it should also have cross-device accessibility with smartphones, tablets, and desktops.
-
Secure Payment Gateway
Payment Method: To ensure secure transactions, it must offer support to various payment gateways for consultation and health care services.
Benefits of Telemedicine Software Solutions for Patients and Health Care Providers

- Accessibility: Redeem healthcare services at any time and place
- Reduced Waiting Hours: No long queues in clinics and hospitals
- Economy: Save on travel expenses and consultation fees.
- Emergency Response: Get help right where you are in the event of an emergency.
- Privacy and Confidentiality: Enabling patients’ data protection via secured platforms.
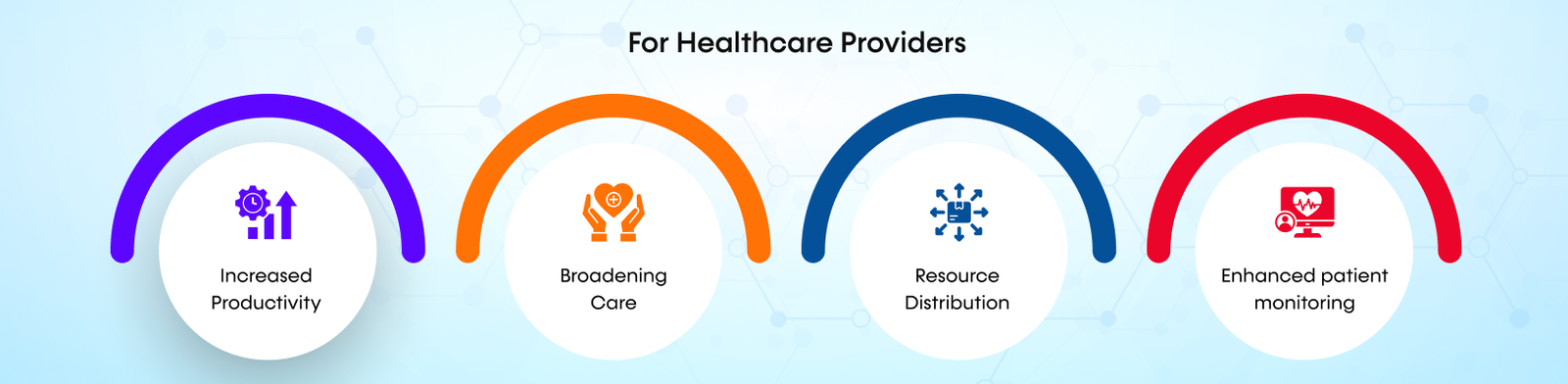
- Increased Productivity: Consult more patients through teleconsultations.
- Broadening Care: Provide service to rural or under-served populations.
- Resource Distribution: Make the task of getting to health facilities easier.
- Enhanced patient monitoring: Manage chronic diseases & Follow-ups on time by practising telemedicine
The digital world of healthcare is combining emerging technologies with AI, IoT, and Blockchain through telemedicine software solutions. These solutions enable:

- Health AI: Algorithms driven by machine learning help doctors diagnose diseases with greater accuracy.
- RPM: RPM is Remote Patient Monitoring, and it uses real-time health data obtained from the patient through devices with wearables, thus allowing remote monitoring.
- Cryptography To Secure Medical Data: Urges an enhanced secure communication system to ensure the protection of patient data and also check deceptive activity.
- Cloud-based Telemedicine Platforms: Provide scalable and cost-efficient healthcare solutions.
Despite having these essential benefits, telemedicine apps come with a few challenges that need to be used proficiently:

- Regulatory Compliance: The apps must adhere to data privacy regulations such as HIPAA and GDPR.
- Data Security Challenges: Strong encryption and cybersecurity protocols are essential to protect data from hacks and security breaches.
- Limited Digital Literacy: Patients, especially the older ones, may not be charted for telemedicine platforms.
- Issues With Internet Connectivity: The Pitfall Of Virtual Consultation
Conclusion
Telemedicine apps – the how of modern healthcare in which treatment is within reach, no travelling to your physician anymore. Apart from this, the future of digital healthcare is going to be even more innovative and accessible with the introduction of telemedicine software solutions.
However, wish to create a telemedicine app with all the features? About Emed HealthTech: Have you ever thought you could use a mobile application to track health concerns and detect health issues in your patients? Contact us today to establish that stable and secure telemedicine solution just for you!