Telemedicine as a concept dates as far back as the 1950s when healthcare providers used technology to deliver healthcare services. It has been holding global attention for a couple of years now. Since the COVID pandemic shook the world and confined us to our homes, people turned to technology to make telemedicine happen. Telehealth appointments witnessed a remarkable increase of 154% compared to the same period in 2019.
Technology is advancing as time passes by. With 5G connectivity, IoT, and wearable tech making telemedicine more accessible and democratic, it is changing the way we interact with the medical industry.
In this article, we examine the role that telemedicine apps play in modern healthcare services. We also look at their benefits, challenges, applications, and future implications.
The Evolution of Telemedicine Apps
Telemedicine owes much of its popularity to the pandemic times. This is in reference to the COVID-19 pandemic and the resulting surge in the use of these tools. We can safely look at the timeline of telemedicine app evolution in terms of the pandemic.
With that perspective, let us look at how this tech has evolved…
Telemedicine in Pre-Pandemic Era
Before the pandemic, telemedicine apps existed even though they were not widely used. It was also not adopted as much by healthcare providers.
The existing apps mainly functioned as basic video chat platforms with limited medical features. The regulations surrounding the use of such platforms were not very favorable to the cause. It restricted the coverage, as well as limited reimbursement options for virtual care services. Telemedicine apps were only seen as supplementary to traditional in-person visits. They could not be thought of as a replacement.
Telemedicine in Pandemic Era
The onset of the pandemic marked a significant turning point for telemedicine app development and use. The COVID-19 lockdown forced people indoors. Social distancing became a norm. It was then that telehealth experienced a rapid and substantial surge in usage.
Healthcare providers were quick to adopt telehealth as a means to provide care while sticking to safety protocols. Regulatory changes played a crucial role in this shift too. Healthcare regulatory compliances now expanded coverage and reimbursement to include telehealth services for patients covered by Medicare and Medicaid.
In response to the growing demand, telemedicine app developers rolled out advanced features that went beyond simple video calls. These apps evolved to enable remote examinations, streamline care coordination, offer patient education, and manage chronic diseases from a distance. As consumers adapted to the new normal, their comfort level with using telehealth apps to access medical care from the comfort of their homes increased.
Telemedicine in Post Pandemic Era
As the pandemic gradually receded, the impact of telemedicine became lasting. Telemedicine apps have now moved from a niche concept to a mainstream healthcare solution. Systems like the electronic health record (EHR) are a part of these apps.
Many healthcare providers have incorporated telehealth as a permanent component of their clinical workflow. Regulatory support has become favorable, reinforcing its use and reimbursement of telemedicine services.
Furthermore, telemedicine app developers have incorporated advanced technologies to make it more accessible and effective. Technologies like Artificial Intelligence (AI), Remote Patient Monitoring (RPM), and wearable devices increase the capabilities and value of their applications.
With consumer expectations transformed, the demand for virtual care options and mobile health management has become an integral part of the healthcare landscape.
Challenges and Benefits of Telemedicine apps
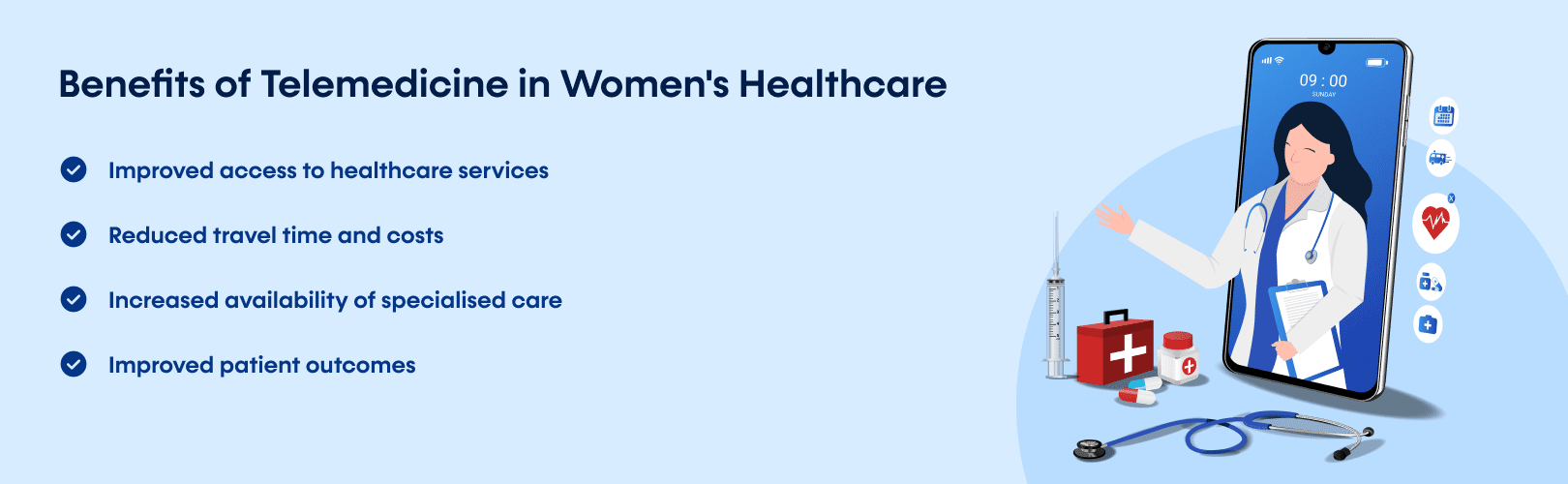
Telemedicine became popular in the first place because of the advantages it offered. Here are some of them:
–> Convenience and Accessibility: Telemedicine apps provide patients with convenient access to healthcare services, eliminating the need for unnecessary travel and wait times.
–> Reduced Transmission Risk: Telemedicine lowers the risk of communicable disease transmission, a crucial factor in pandemic-like scenarios.
–> Efficiency and Time Savings: Telemedicine reduces overall time taken for visits, benefiting both patients and healthcare providers.
There are challenges to using Telemedicine as well. Some of them are:
–> Challenges in Replacing Physical Examinations: Telemedicine apps offer numerous advantages, but it has one major limitation. It does not allow for a physical examination, which is an important part of a medical diagnosis.
–> Accessibility and Device Limitations: Device and network availability can become a roadblock to universal access to telemedicine services.
–> Technical Challenges: Network disruptions and technical difficulties can impede the effectiveness of telemedicine apps.
Overcoming Challenges for Widespread Adoption of Telemedicine
If telemedicine has to reach its potential and change the face of the medical industry, it has to overcome several challenges. And these challenges need strategic solutions.
Healthcare policies have changed in recent times to accommodate reimbursement of telemedicine services. It has been pivotal in driving its adoption.
However, addressing licensing and regulatory barriers is equally vital to extending the reach of telemedicine services. To gain patient acceptance and confidence, it is important to maintain the same high level of quality in telemedicine services as in traditional in-person care.
It is important to address the security risks associated with this tech. Healthcare involves a lot of sensitive info about a patient. The provider has to ensure the utmost data privacy and security. There should be strict enforcement of the regulations like HIPAA. It is essential in building and retaining patient trust in telemedicine apps.
Collectively, overcoming these challenges is essential to realizing the full potential of telemedicine and ensuring its integration as a reliable and effective healthcare solution.
Future Perspectives and Growth of Telemedicine and Telehealth
Here is what we can expect from Telemedicine and Telehealth in 2023 and beyond. Three major factors are fueling the growth of the telemedicine industry. Let us look at each of them in detail.
1. Need for Convenience
Firstly, the aging population and the increasing consumer preference for easier and more accessible healthcare services are acting as strong drivers. Older individuals require more frequent medical attention and visits.
However, mobility is an issue they face along the way. Telemedicine offers them an alternative to getting medical care from the comfort of their home.
For instance, elderly patients with chronic conditions like diabetes can now monitor their health parameters using wearable devices and telemedicine apps. This reduces the need for frequent visits to medical facilities.
2. Technological Advancement
Secondly, continuous technological advancements are shaping the evolution of telemedicine apps. These advancements are making apps more complex and more accessible to people. From AI-powered diagnostic tools to real-time remote patient monitoring, healthcare delivery is becoming more accurate and comprehensive.
For instance, advanced telemedicine apps can now analyze medical images, such as X-rays, and provide immediate insights, expediting the diagnostic process.
3. Connectivity
This is the era of 5G and ultra-high-speed data transmissions. Healthcare is also showing signs of change in this regard.
Moreover, the rise of the “connected health” model is ushering in a positive shift, powered by these telehealth apps. This model empowers patients to actively engage in their healthcare journey through features like health tracking, medication reminders, and personalized health recommendations.
It also promotes self-management and timely interventions. The connected health model reduces hospital stays and improves overall health outcomes.
For example, patients recovering from surgery can use telemedicine apps to receive post-operative care instructions, reducing the need for prolonged hospital stays.
Measures for the Future of Telemedicine Development
We need to consider the sustainable and scalable growth of telemedicine apps. It takes strategic planning, including integration with existing healthcare systems, to make a robust infrastructure that can handle the traffic load. Scalability and data security are important factors to consider when it comes to growth.
Additionally, healthcare professionals need effective training to maximize the potential of these apps and provide quality virtual care.
By addressing these elements, the telemedicine industry can confidently expand its reach while maintaining high standards of service quality.
Build a Telemedicine Platform to Future-Proof Your Healthcare Service
Telemedicine app development services have emerged as a transformative force in modern healthcare. One cannot overstate their role in empowering the modern healthcare industry. Partnering with a telemedicine app development company can be a transformative force for any healthcare facility.
To explore the full potential of telemedicine apps, choose reliable telemedicine app developers like EMed HealthTech. As a trusted telemedicine app development company, we have helped many clients achieve their desired results with custom healthcare applications.
If you’re looking to embrace telemedicine and adapt your business to the demands of the digital age, get in touch with us. We’ll be delighted to discuss your project needs.