As our world hurtles forward in a whirlwind of technological advancements, our expectations for healthcare have evolved too. There is a demand for convenient and accessible healthcare solutions. Telemedicine has risen to the challenge and caters to the changing needs of the time. Healthcare providers now simply need only choose what kind of white label telemedicine platform they are ready to offer.
Imagine having the power to create your very own telemedicine platform customized to meet the specific needs of your patients and healthcare providers. With a well-developed white label telemedicine app, you can do just that and more.
In this article, we will explore the key features and functionalities of telemedicine platform, the development and implementation process, and the future trends and opportunities they present. We will also address the challenges and considerations involved in the telemedicine development process, ensuring that you are well-equipped to navigate this transformative journey.
Understanding White Label Telemedicine Platform

But before we dive into the nitty-gritty, let’s take a moment to appreciate the soaring demand for telemedicine services. The COVID-19 pandemic acted as a catalyst, accelerating the adoption of telemedicine and highlighting its indispensable role in delivering healthcare remotely.
According to a study, telemedicine software use increased considerably during the COVID-19 pandemic, with lower use in communities with higher poverty rates. They found that 30.1% of all outpatient visits were conducted via telemedicine software during the pandemic and that the number of weekly visits increased twenty-three-fold compared to pre-pandemic appointments.
People now seek the convenience of virtual doctor consultations, saving time and effort by avoiding crowded waiting rooms. Telemedicine software has become a lifeline, connecting patients with healthcare professionals, irrespective of physical distance.
What is a White label Telemedicine App?
A white label telemedicine app is a software application allowing healthcare providers to offer telemedicine services to their patients under their brand. Unlike custom-built apps, white label apps are pre-developed and ready-to-use solutions that can be easily customized and rebranded to match the provider’s identity. These apps typically come with essential features such as appointment scheduling, video/audio consultations, secure messaging, and electronic health records (EHR) integration.
Healthcare providers can quickly establish a virtual presence, enabling patients to access medical consultations remotely. The app facilitates seamless communication between patients and healthcare professionals, allowing for real-time consultations, diagnoses, and treatment plans. It also provides a secure platform for sharing medical records and prescriptions.
White label telemedicine apps offer several advantages, including reduced development costs, faster time-to-market, and a tested user experience. These apps enable healthcare providers to leverage the power of telemedicine technology without the need for extensive technical knowledge or resources, ultimately enhancing patient access to healthcare services and improving overall healthcare delivery.
What sets apart white label telemedicine apps from custom-built solutions?
Custom telemedicine solutions differ in terms of their development process and customization options. A telemedicine app is a pre-built, ready-to-use solution that can be easily customized and rebranded to match a healthcare provider’s brand identity.
In contrast to readymade software, custom-built software involves developing an app from scratch, tailored specifically to the provider’s unique requirements.
While white label apps offer a faster and more cost-effective option, custom-built solutions provide greater flexibility and control over the app’s features and design. Healthcare providers must consider their specific needs, resources, and time constraints when deciding between a white label telemedicine app and a custom-built solution for their telemedicine software.
Key Features and Functionality of Telemedicine Platform
1. Appointment booking and scheduling
White label platforms offer user-friendly interfaces for easy appointment management, including calendars, reminders, and rescheduling options.
2. Seamless doctor-patient communication
Real-time, secure messaging systems enable convenient communication between doctors and patients for consultations and inquiries.
3. Video, audio, and chat consultations
White label platforms support various consultation modes, accommodating patient preferences and medical conditions.
4. Electronic health records and data security
Integration with EHR systems provides access to patient history while stringent security measures protect sensitive data.
5. Integration with payment gateways
Secure payment gateways simplify transactions, allowing patients to make payments within the platform.
6. Customization for branding and user interface
Branding options, logos, and personalized interfaces create a consistent and tailored experience for patients.
Reasons You Should be Investing in a White Label Telemedicine Platform
Investing in a telemedicine solutions offers numerous advantages to the healthcare provider. Here are some of the reasons you should look for a telemedicine platform development:
1. Cost-effectiveness
White label telemedicine platforms offer a cost-effective solution compared to custom-built options, as they eliminate the need for extensive development and coding from scratch.
2. Time-saving
Investing in a white label telemedicine platform allows you to launch your telemedicine services quickly without the lengthy development process, significantly reducing time-to-market.
3. Customizability
White label platforms provide the flexibility to customize and brand the app according to your organization’s identity, ensuring a seamless user experience for both patients and healthcare providers.
4. Proven functionality
White label telemedicine platforms are already tested and refined, ensuring reliable performance and a user-friendly interface, backed by their successful implementation in the market.
5. Scalability
With a white label solution, you can easily scale your telemedicine services as your user base grows without worrying about technical limitations or infrastructure constraints.
6. Enhanced patient care
A white label telemedicine platform allows for efficient remote consultations, enabling patients to access healthcare services conveniently and receive timely medical assistance regardless of their location.
7. Competitive advantage
Investing in a white label telemedicine platform gives your organization a competitive edge in the evolving healthcare industry, meeting the increasing demand for accessible and convenient telemedicine services.
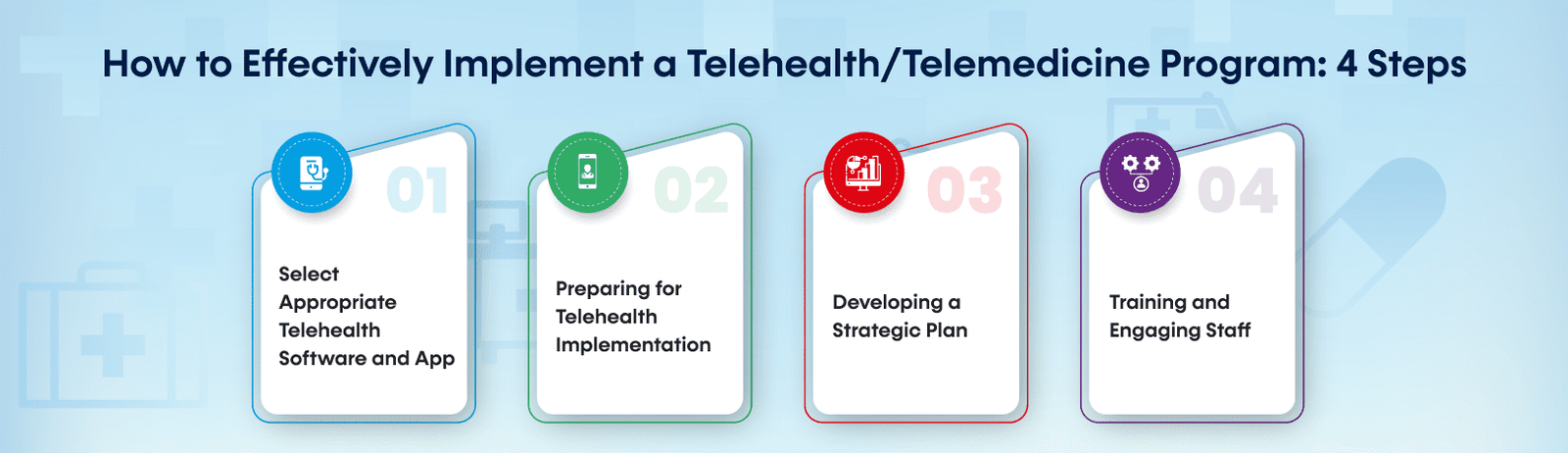
Developing a White Label Telemedicine Platform
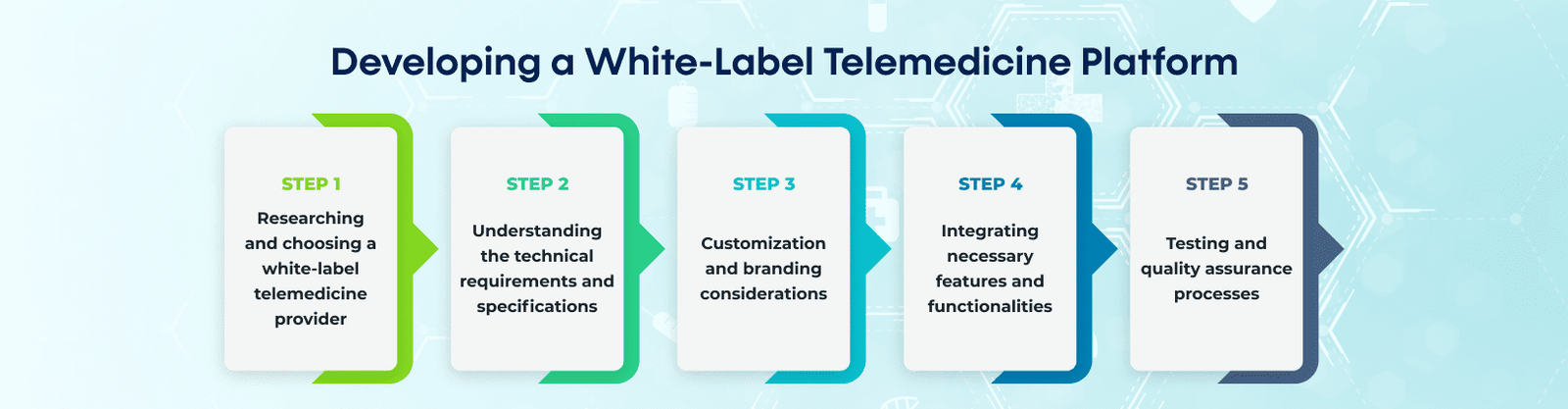
Let us look into the process of creating a white label telemedicine app for your healthcare service.
Step 1: Researching and choosing a white label telemedicine provider
The first step in developing a white label telemedicine platform is to research and select a reliable and reputable white label telemedicine provider. Evaluate different providers based on factors such as their track record, customer reviews, available features, scalability, and pricing plans. Consider your specific requirements and choose a provider that aligns with your business goals.
Step 2: Understanding the technical requirements and specifications
Once you’ve chosen a provider, it’s essential to understand the technical requirements and specifications of the white label platform. This includes determining compatibility with different devices and operating systems, network requirements, and integration capabilities with other systems or databases. Collaborate with your IT team or the provider’s technical support to ensure a smooth implementation.
Step 3: Customization and branding considerations
Customization options should be explored to create a unique and branded telemedicine software. Consider aspects like logo placement, color schemes, fonts, and overall user interface design. Ensure that the platform reflects your organization’s brand identity and provides a seamless user experience for patients and healthcare providers.
Step 4: Integrating necessary features and functionalities
Work closely with the white label provider to integrate the required features and functionalities into the platform. This may include appointment scheduling, secure messaging, video consultations, electronic health records, payment gateways, and other specific requirements based on your telemedicine services. Ensure that the platform supports essential functionalities for both patients and healthcare professionals.
Step 5: Testing and quality assurance processes
Before launching the platform, rigorous testing and quality assurance processes are crucial. Conduct thorough testing to identify and fix any bugs, ensure proper functionality, and verify the security of patient data. Test the platform from different devices and networks to ensure a consistent and reliable user experience. Perform comprehensive quality checks to guarantee that the platform meets industry standards and regulatory compliance.
Future Trends and Opportunities in White Label Telemedicine Platforms

The future of white label telemedicine platforms holds exciting possibilities for innovation and growth. Here is what we can expect from Telemedicine and Telehealth in 2023 and in the future. Advancements in artificial intelligence and machine learning are poised to enhance the capabilities of these platforms, enabling personalized treatment plans and more accurate diagnoses. Integration with wearable devices and remote monitoring tools will enable continuous health tracking, further enhancing the remote healthcare experience. Moreover, telemedicine services are expanding beyond primary care, encompassing specialties and subspecialties, opening up new avenues for telemedicine software providers. The increasing demand for telemedicine services presents significant opportunities for platform providers to meet the evolving needs of patients and healthcare professionals alike. By staying at the forefront of these trends, white label telemedicine platform providers can shape the future of healthcare delivery.
Final Words
Developing a white label telemedicine platform allows healthcare providers to meet the growing demand for convenient and accessible healthcare services.
With the ability to customize and brand the platform, healthcare providers can establish their virtual presence quickly and provide seamless communication between doctors and patients. By leveraging these platforms, healthcare providers can revolutionize the way healthcare is delivered, ensuring accessibility, convenience, and quality care for all.
If you’re ready to harness the power of white label telemedicine platforms, EMed HealthTech – a healthcare app development company is here to help.
With our expertise in building customizable and branded telemedicine solutions, we can empower your healthcare organization to deliver convenient and accessible healthcare services.
Contact us today to explore the possibilities!